In the recent medical news, the USPSTF (an organization that that evaluates evidence and makes certain medical recommendations) is drafting a revision to its guidelines for primary prevention of cardiovascular disease with statins, which are medications such as Simvastatin (Zocor) and Atorvastatin (Lipitor). The new recommendation is that people ages 40-75 who are at high risk for cardiovascular disease should take this type of medication to prevent heart attacks.
Because patients (and even doctors) do not have time to go through the medical literature themselves, we depend on organizations like the USPSTF to do the work of reviewing the literature and make evidence-based recommendations for the public. Once this happens, the recommendation is accepted as the truth and ingrained into the standard of care of medicine.
My purpose in writing this article is not to argue for or against this recommendation or to argue for or against statins in general. Whether or not an individual person should take a statin medication should be an individualized decision that patients should be able to have with their personal physician. My purpose rather is to show that the “recommendation” should not be taken as gospel, that we should continue to be open-minded about scientific evidence, and that the benefits of statins in general are probably perceived to be greater than they actually are.
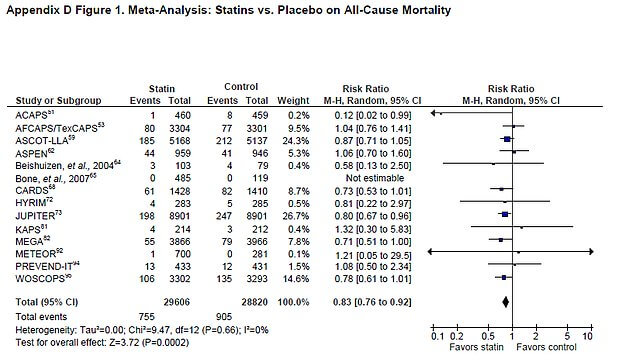
Let us take an in-depth look specifically at the effect of statins on all-cause mortality for primary prevention (those who have not had a previous cardiovascular event). The USPSTF has analyzed all of the relevant studies that look at this in order to form their recommendation:
Now let us compare this to a similar study: a meta-analysis done in 2010 that was published in the Archives of Internal Medicine. A meta-analysis is also a combined review of the available literature on a certain question:
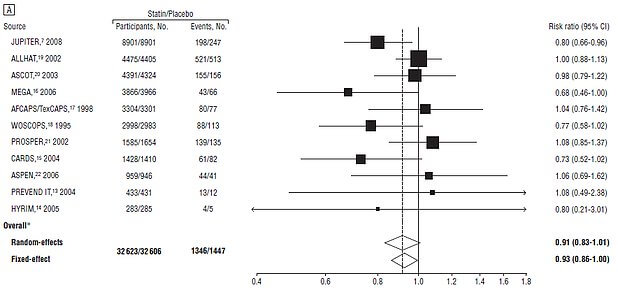
To be clear, there were no new studies done since 2010. Both studies looked at the exact same body of evidence. The conclusions of each of the following papers are below:
USPSTF: Statins reduce all-cause mortality in primary prevention of cardiovascular disease for those at high risk.
Archives of Internal Medicine: “This literature-based meta-analysis did not find evidence for the benefit of statin therapy on all-cause mortality in a high-risk primary prevention set-up”
How is this possible? How can two studies looking at the same question that are looking at the exact same body of evidence arrive at the opposite conclusion. The answer is that there is a lot of opinion and judgment that goes into producing a meta-analysis. For example, the two studies made slightly different decisions about which studies to include or exclude for various reasons:
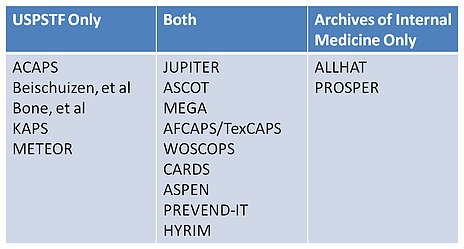
Small technicalities in methodology can make huge impacts on the final conclusion of the analysis, which has tremendous consequences for what patients and doctors believe is the right thing to do. Let us for a moment, pretend that both studies achieved statistical significance. These are the combined (unweighted) results of the two studies:
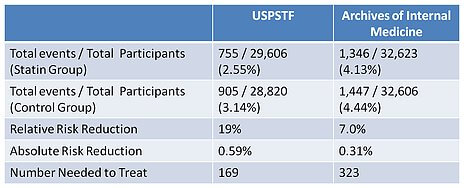
Number needed to treat is the number of people needed to be treated for one person to be affected. So the data from these studies shows that we have to treat with statin medication somewhere between 169 and 323 people in order to save one person’s life. When stated this way, the benefits of statins seem much less impressive compared to the perceived confidence of an official USPSTF recommendation.
This potential benefit needs to be balanced with the risks of taking this medication:
Gastrointestinal: Diarrhea (7% to 14%)
Neuromuscular & skeletal: Arthralgia (9% to 12%)
Respiratory: Nasopharyngitis (13%)
Cardiovascular: Hemorrhagic stroke (2%)
Central nervous system: Insomnia (5%)
Endocrine & metabolic: Diabetes mellitus (6%)
Gastrointestinal: Nausea (7%), dyspepsia (6%)
Genitourinary: Urinary tract infection (7% to 8%), cystitis (interstitial; Huang 2015)
Hepatic: Increased serum transaminases (≤2%)
Neuromuscular & skeletal: Limb pain (9%), myalgia (4% to 8%), musculoskeletal pain (5%), muscle spasm (4% to 5%)
Respiratory: Pharyngolaryngeal pain (3% to 4%)
<2% (Limited to important or life-threatening): Abdominal pain, abnormal hepatic function tests, alopecia, anaphylaxis, anemia, angioedema, anorexia, cholestasis, cholestatic jaundice, cognitive dysfunction (reversible), confusion (reversible), depression, elevated glycosylated hemoglobin (HbA1c), epistaxis, eructation, erythema multiforme, gynecomastia, hematuria, hepatic failure, hepatitis, hyperglycemia, hypoesthesia, increased creatinine phosphokinase, increased serum alkaline phosphatase, increased serum glucose, jaundice, joint swelling, muscle fatigue, myasthenia, myopathy, myositis, neck stiffness, nightmares, pancreatitis, paresthesia, peripheral edema, peripheral neuropathy, rhabdomyolysis, rupture of tendon, Stevens-Johnson syndrome, thrombocytopenia, toxic epidermal necrolysis
From a biochemical point of view, we know that statin medication inhibit the synthesis of CoQ10 and Vitamin K2.
Coenzyme Q10 is involved in energy production, so they effect heart health as well, as the heart needs to produce a large amount of energy to function. Deficiency causes chest pain, heart failure, and high blood pressure, but also aging, Alzheimer’s and cognitive dysfunction, Parkinson’s, metabolic dysfunction, and diabetes.
Vitamin K2 is involved in calcium regulation, making sure that calcium goes into the bones and away from the heart and blood vessels. Thus, a Vitamin K2 deficiency can contribute to osteoporosis, heart disease, and high blood pressure.
When taking all of this into account and putting everything in perspective the decision is likely not as obvious. This is why each individual person should have an informed discussion with their doctor about the risks and benefits of statins. Together, you will be able to make the decision that is right for you based on your risk and values.
I want to emphasize that I am not anti-medication or anti-statin. I have many patients for whom I strongly believe the benefits of medication outweigh the risks. But what we need to understand as a society is that science is not as certain as we think it is, and despite general recommendations from our government task force, we need to continue to be critical about the scientific literature and continue to make individualized decisions.

