What do asthma, dry eyes, and psoriasis all have in common? They are all completely different things, right? Well, it is true that they are all different in terms of their specific pathology, target organ system, and prevalence in the population. However, from a functional perspective, they are all the same thing: chronic inflammation and immunologic dysfunction. In our opinion, it is more useful to categorize things by their functional imbalances, not by the minutiae of their pathology. Thus, we would tend to look at these types of issues on a spectrum that depicts the degree of immunological dysfunction (see Figure below).
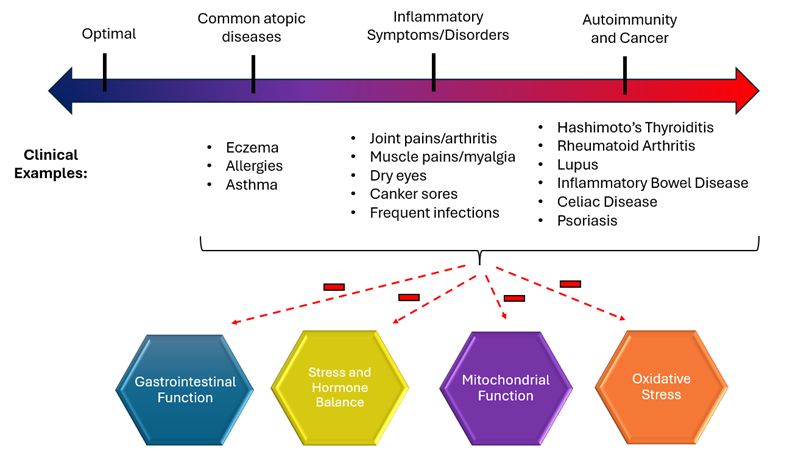
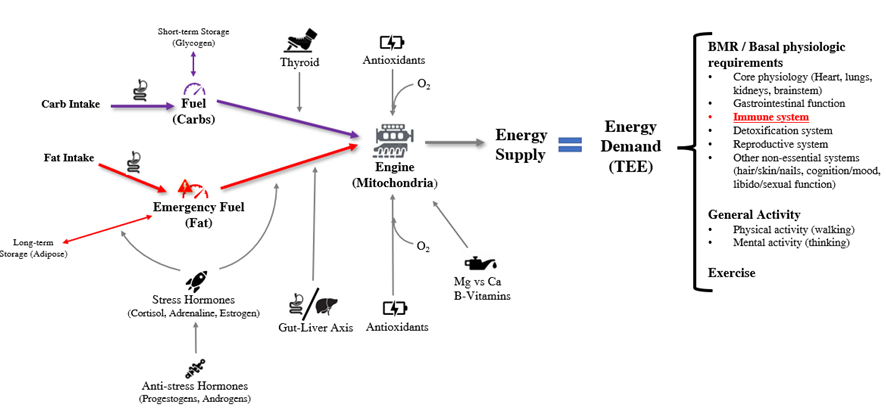
The term inflammation refers to the body’s response to infection or damaged tissue. It can be thought of as fire. For example, consider the situation in which an individual sprains their ankle. What happens? It gets red, hot, swollen, and painful. The body has essentially set that joint on fire in order to break down the damaged tissue and then rebuild new and healthy tissue. Thus, acute inflammation is a normal part of how our body functions. However, a more significant functional problem ensues when the inflammation becomes chronic and systemic. In this case, the whole body is on fire. This fire then creates an increased energetic demand (stress activation), damages the mitochondria (engine malfunction), affects the core functions of the gastrointestinal tract (promotes maldigestion and dysbiosis), and feeds oxidative stress.
Inflammation is managed by the immune system. Thus, the ideas of chronic inflammation and immune system dysfunction are intricately connected. From a functional perspective, they are the same thing. When the joints of your fingers start hurting and your healthcare provider tells you that you have “arthritis,” you feel the inflammation in those joints, but what is really happening is that immune system in those areas is overactive. This is true regardless of whether you specifically test positive for Rheumatoid Arthritis or not. For the remainder of this article, we will use the terms “inflammation” and “immune system dysfunction” interchangeably.
Causes of Inflammation / Immune System Dysfunction and the Importance of Food Sensitivities
Please see our article Functional Medicine Approach to Autoimmunity for a review of the causes of immune system dysfunction and the particular importance of food sensitivities.
Objective Evidence of Inflammatory / Immune System Dysfunction
Clinical symptoms should be combined with objective evidence to determine how significant the immunologic dysfunction is. Objective evidence, however, is complex because different issues can affect different aspects of the immune system. For example, we often see patients with a normal C-Reactive Protein (CRP) level even though it is clear that they are highly inflamed. Additionally, there is lack of consensus on how to approach testing for autoantibodies, which can potentially lead to misclassification due to lack of testing. For example, the medical condition known as POTS (Postural Orthostatic Tachycardia Syndrome) is not generally thought to be an immunologic condition; however, studies show that this condition is associated with autoantibodies against adrenergic receptors, muscarinic acetylcholine receptors, and other structural cardiac proteins.
Objective evidence for immunologic dysfunction includes:
- Elevated C-Reactive Protein (CRP)
- Abnormal White Blood Cell (WBC) counts
- Elevated autoantibody levels
- Elevated antibodies against various foods (abnormal Food Sensitivity Testing)
- Elevated fecal calprotectin
- Abnormal cytokine levels (interleukins, TGF-beta, IFN-gamma, etc.)
Cancer is Also an Immunologic Dysfunction
While cancer is not an autoimmune condition, it does have an important relationship with the immune system. As opposed to autoimmunity, in which the immune system inappropriately attacks healthy cells, cancer pathophysiology involves failure of the immune system to attack defective/mutated cells, allowing them to inappropriately grow and divide.
Minimizing Inflammatory / Immunologic Dysfunction is Crucial for Overall Bioenergetic Optimization
As mentioned above, inflammation/immune system imbalance represents a chronic fire that damages multiple aspects of the metabolic system. Not only does it represent an energetic demand on the system, which promotes chronic stress activation, but studies show that it directly damages the mitochondrial/engine function, leading to a low energy supply. On top of that, inflammation may damage other specific aspects of the system’s bioenergetic function. For example, gastrointestinal inflammation may lead to malabsorption and fuel deficiency, thyroid inflammation leads to primary hypothyroidism, liver inflammation leads to poor bile flow and lack of GLP-1 secretion, etc. Thus, fixing this problem is often critically important for overall bioenergetic optimization.
For those interested in learning more about the connection between immune system dysfunction and other functional imbalances in more detail, consider reading the relevant sections in our manual.

